Tourette syndrome (TS) is a neurological disorder that typically begins in childhood and is characterized by repetitive, involuntary movements and vocalizations called tics. Tics can range from simple, brief movements such as eye blinking or shoulder shrugging to more complex actions such as facial grimacing or repeating words or phrases.
Tourette syndrome is often accompanied by other conditions such as attention-deficit/hyperactivity disorder (ADHD) and obsessive-compulsive disorder (OCD). The exact cause of Tourette syndrome is not fully understood, but it is believed to involve both genetic and environmental factors. While there is no cure for Tourette syndrome, treatment can help manage symptoms and improve quality of life. This may include medications, behavioral therapy, or a combination of both.
What treatment can help manage tourettes?
Treatment for Tourette syndrome is based on the individual’s specific symptoms and needs. There is no cure for Tourette syndrome, but treatment can help manage symptoms and improve quality of life. Here are some common treatments that can help manage Tourette syndrome:
Medications: Certain medications, such as antipsychotics, alpha-adrenergic agonists, and dopamine-depleting agents, can help control tics and other symptoms associated with Tourette syndrome.
Antipsychotics, also known as neuroleptics, are a class of medications primarily used to treat psychotic disorders such as schizophrenia, bipolar disorder, and severe depression with psychotic features. They work by blocking or reducing the effects of dopamine and other neurotransmitters in the brain that are involved in regulating mood, thought processes, and behavior.
There are two main types of antipsychotics: typical and atypical. Typical antipsychotics, also called first-generation antipsychotics, were developed in the 1950s and 1960s and include medications such as haloperidol and chlorpromazine. Atypical antipsychotics, also called second-generation antipsychotics, were developed in the 1990s and include medications such as risperidone, olanzapine, and quetiapine.
Antipsychotics are typically taken orally in pill or liquid form, but some are available as injectable formulations. The choice of medication and route of administration will depend on the individual’s symptoms, medical history, and preferences.
Antipsychotics can have significant side effects, including weight gain, sedation, movement disorders such as tremors and stiffness, and metabolic changes such as increased blood sugar and cholesterol levels. Long-term use of antipsychotics may also increase the risk of developing tardive dyskinesia, a condition characterized by involuntary movements of the face, tongue, and limbs.
It’s important to work closely with a healthcare professional when taking antipsychotics to monitor for side effects and adjust the dosage or medication as needed. Antipsychotics should not be stopped abruptly without medical supervision, as this can lead to withdrawal symptoms and worsening of symptoms.
Behavioral therapy: Behavioral therapy can help individuals with Tourette syndrome learn how to manage their tics, reduce stress, and cope with any associated conditions such as ADHD or OCD. Some types of behavioral therapy that may be helpful include habit reversal therapy, cognitive-behavioral therapy, and relaxation techniques.
Behavioral therapy is a type of psychotherapy that focuses on changing patterns of behavior that may be causing problems or distress in an individual’s life. It is based on the principles of learning theory and is designed to help individuals learn new skills and behaviors to improve their mental health and well-being.
Behavioral therapy is often used to treat a variety of mental health conditions, including anxiety disorders, depression, obsessive-compulsive disorder (OCD), and post-traumatic stress disorder (PTSD). It can also be helpful for managing symptoms of other conditions, such as Tourette syndrome and substance use disorders.
There are several types of behavioral therapy, including:
Cognitive-behavioral therapy (CBT): CBT is a type of therapy that focuses on identifying and changing negative thought patterns and beliefs that may be contributing to mental health problems. It combines cognitive therapy, which focuses on changing thoughts and beliefs, with behavioral therapy, which focuses on changing behaviors.
Dialectical behavior therapy (DBT): DBT is a type of therapy that focuses on teaching individuals skills to manage intense emotions, improve relationships, and regulate behavior. It is often used to treat borderline personality disorder.
Exposure therapy: Exposure therapy is a type of therapy that involves gradually exposing an individual to feared situations or objects in a controlled environment to help them overcome anxiety or phobias.
Applied behavior analysis (ABA): ABA is a type of therapy that is often used to treat autism spectrum disorders. It focuses on teaching new behaviors and skills through positive reinforcement and systematic desensitization.
Behavioral therapy is typically delivered by a trained mental health professional, such as a psychologist or licensed clinical social worker. It can be delivered in individual or group settings and may involve homework assignments and other exercises to reinforce new behaviors and skills.
Behavioral therapy is often an effective treatment option for mental health conditions, particularly when used in combination with other treatments such as medication or supportive therapy.
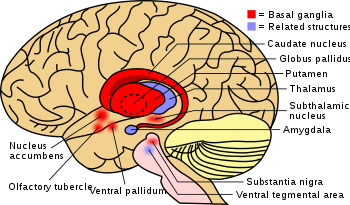
Deep brain stimulation: Deep brain stimulation (DBS) is a surgical procedure in which electrodes are implanted in the brain to stimulate certain areas that are involved in controlling movement. This treatment may be helpful for individuals with severe Tourette syndrome who do not respond to other treatments.
Deep brain stimulation (DBS) is a surgical procedure that involves implanting electrodes in specific areas of the brain to treat a variety of neurological and psychiatric conditions. It is a relatively new treatment and is typically reserved for individuals who have not responded to other treatments or who experience severe symptoms that significantly affect their quality of life.
During the DBS procedure, electrodes are implanted into the brain and connected to a small device called a neurostimulator, which is implanted under the skin near the collarbone. The neurostimulator sends electrical impulses to the brain through the electrodes, which can help regulate abnormal brain activity and improve symptoms.
DBS has been used to treat a variety of conditions, including Parkinson’s disease, essential tremor, dystonia, and obsessive-compulsive disorder (OCD). It is also being studied as a potential treatment for other conditions, such as epilepsy, depression, and Tourette syndrome.
DBS is typically reserved for individuals who have not responded to other treatments or who experience severe symptoms that significantly affect their quality of life. It is important to note that DBS is a complex and invasive procedure that carries significant risks, including infection, bleeding, and neurological complications. It also requires careful monitoring and adjustment by a trained healthcare professional to ensure optimal outcomes.
Overall, DBS has the potential to be an effective treatment option for certain individuals with neurological and psychiatric conditions, but it is not a cure and may not be suitable for everyone. It is important to consult with a healthcare professional to determine whether DBS is an appropriate treatment option and to discuss the potential risks and benefits.
Supportive therapies: Other supportive therapies, such as occupational therapy or speech therapy, may be helpful for individuals with Tourette syndrome to improve motor skills, speech, and communication.
Supportive therapies are a group of interventions that are designed to provide emotional, psychological, and social support to individuals who are experiencing a wide range of difficulties, including mental health conditions, chronic illnesses, and life-changing events. The goal of supportive therapies is to improve an individual’s quality of life, promote emotional well-being, and enhance their ability to cope with challenges.
There are several types of supportive therapies, including:
Counseling or psychotherapy: Counseling or psychotherapy involves talking to a trained mental health professional about issues or challenges that may be affecting an individual’s emotional and psychological well-being. Counseling may be delivered in individual or group settings and can focus on a range of issues, including depression, anxiety, relationship problems, and grief.
Support groups: Support groups are groups of individuals who share a common experience or challenge, such as living with a chronic illness or caring for a loved one with a disability. Support groups provide a safe and supportive environment for individuals to share their experiences, feelings, and challenges and to receive emotional and practical support from others who are going through similar experiences.
Mind-body therapies: Mind-body therapies, such as meditation, yoga, and tai chi, are practices that focus on the connection between the mind and body. These therapies are designed to reduce stress and promote relaxation and can be helpful for managing a variety of conditions, including chronic pain, anxiety, and depression.
Art therapy: Art therapy involves using art materials and creative expression to explore emotions, reduce stress, and promote well-being. Art therapy can be helpful for individuals who have difficulty expressing themselves verbally or who find it difficult to engage in traditional talk therapy.
Supportive therapies can be used in conjunction with other treatments, such as medication or behavioral therapy, to enhance their effectiveness. It is important to work with a trained healthcare professional to determine which supportive therapies may be most appropriate and effective for an individual’s specific needs and challenges.
It’s important to work closely with a healthcare professional to develop a treatment plan that is tailored to the individual’s specific needs and symptoms.